Introduction
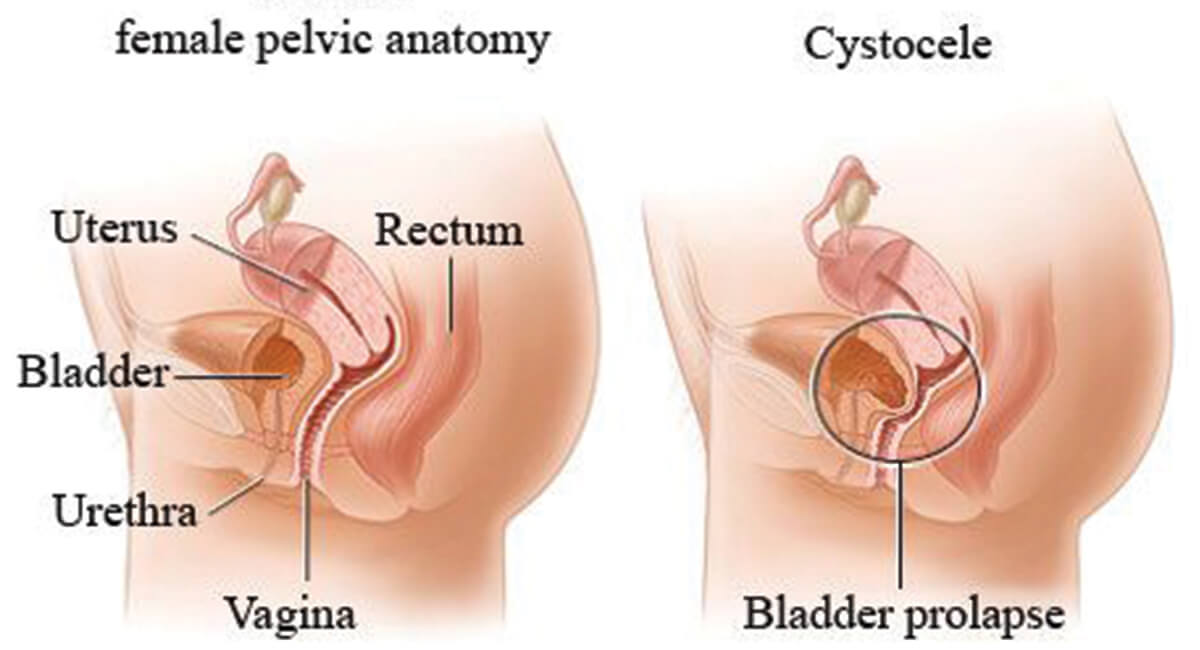
Prolapse is the descending of organs from their normal position. Pelvic Organ Prolapse occurs when the pelvic muscles and ligaments supporting women’s pelvic organs lose their tonicity. The organs (it could be one or more organs) then descend from their normal position bulging into the uterus, bladder, bowel, or top of the vagina, causing pain. Though not life-threatening, it can cause severe pain and discomfort.
Pelvic floor muscles surround the pelvic organs like a hammock and support the organs to keep them in place and help with normal functioning. When these muscles become weak or damaged (due to an injury), they can no longer support the pelvic organs (which include urinary bladder, uterus, cervix, vagina, and rectum), causing one or more organs to descend from their normal position and bulge into or out of the vagina.
Based on the organ which has descended, various names are given technically:
- ● Cystocele: Prolapse of the urinary bladder.
- ● Urethrocele: Prolapse of the urethra.
- ● Uterine prolapse: Prolapse of uterus.
- ● Enterocele: Bowel prolapse
- ● Rectocele: Prolapse of rectum.
Request an Appointment at Smiles
What are the Causes of Pelvic Organ Prolapse?
- ● Vaginal childbirth: The muscles become weak due to stretching and straining the pelvic muscles during vaginal childbirth. If the patient has had multiple vaginal childbirth, this becomes a risk factor and can cause pelvic organ prolapse in later life stages. But, not everyone with vaginal childbirth will end up with prolapse. However, even if they have never had vaginal childbirth, they can end up with a prolapse.
- ● Long-term pressure on your abdomen: Strain and pressure in the abdomen could be due to obesity or strained bowel movements (chronic constipation). When there is constant pressure on the abdomen, it can lead to weakened pelvic muscles.
- ● Giving birth to a heavy child: When the newborn is above 4 kgs of weight, there is excessive straining of the pelvic muscles.
- ● Aging: More common in older women.
- ● Hormonal changes in menopause: Changes in estrogen levels during menopause increase the risk of prolapse.
- ● External injury: Any external injury damaging the pelvic organs or causing pressure may lead to prolapse.
- ● Hysterectomy: Removal of the uterus may also be a predisposing factor.
What are the Symptoms of Pelvic Organ Prolapse?
- ● Lower backache.
- ● Pain during sexual intercourse.
- ● Pressured feeling in the lower abdomen.
- ● Leakage of urine.
- ● Urine incontinence.
- ● Constipation
- ● Spotting or bleeding from the vagina.
Symptoms depend on which organ has prolapsed. Urine leakage and incontinence occur if the bladder has prolapsed, constipation if the rectum has prolapsed, and lower backache if the small intestine has prolapsed.
How is Pelvic Organ Prolapse Diagnosed?
- ● Intravenous pyelography: An X-ray technique where an injection of contrast material is injected to evaluate your kidneys, ureters, and bladder.
- ● CT scan of the pelvis: Detailed imaging of the area will give a clear picture of the prolapse and which organ has prolapsed. It helps to diagnose and study the prolapse in detail.
- ● Ultrasound: Pelvic ultrasound.
- ● MRI scan: Pelvis MRI.
How is Pelvic Organ Prolapse Treated?
- ● Lose weight: If the patient is obese, then a weight loss will benefit more than one way.
- ● Avoid heavy weight lifting: To prevent further straining of the muscles.
- ● Use laxatives: If the patient is constipated (chronic constipation).
- ● Pelvic exercises: Kegel’s exercise does help to a certain extent. Kegel’s exercise strengthens the pelvic floor muscles and the urinary sphincter. To do this, stop urination midstream, hold urine for 8 to 10 seconds, and release again; this can be done even if you are not urinating and just the act of doing so is enough. Repeat this for three sets of 10 to 15 repetitions; this can be done any time and anywhere.
If the symptoms are severe, then one of the following treatments is an option:
- ● Mechanical treatment: A device called a pessary is inserted into the vagina to support the prolapsed organ.
- ● Surgical treatment: Surgery is done either to repair the injured or damaged muscle and surrounding tissues or to remove the organ as in a hysterectomy. The surgical procedures that use the patient’s tissues and ligament to treat the prolapse include uterosacral ligament fixation, sacrospinous ligament fixation, and McCall culdoplasty. A surgical procedure that uses surgical mesh to treat prolapse through an abdominal incision can also be an option.
What is the Results of Pelvic Organ Prolapse Treatment?
What are the Risk Associated with Pelvic Organ Prolapse Treatment?
- ● Infection
- ● Bleeding
- ● Pain
- ● Problems related to anesthesia
Request an Appointment at Smiles
FAQ's
Can Prolapse get Worse?
Will a Prolapse Recur after Surgery?
What are the Complications in Pelvic Organ Prolapse?
- ● Persistent vaginal bleeding
- ● Pelvic pain
- ● Pain with sex
- ● Urinary incontinence
- ● Problems with bowel movements
What Happens if the Prolapse is left Untreated?
What Activities should I Avoid or do if I have a Prolapse?
- ● Do not do weight lifting
- ● Do not do strenuous work
- ● Do not stand a lot
- ● Drink lots of wate
- ● Eat plenty of fruits and veggies if you have constipation. Also, avoid cheese, a high-fat diet, meat, and fast food
Need Help?
For any Information about our Locations, Doctors or Treatments.
