Listed below are some treatments for Obstructive Defecation Syndrome which range from conservative, non-invasive therapies to surgical interventions with their possible complications.
Conservative treatment:
Dietary treatments and lifestyle changes:
- These changes are generally used as first treatment option.
- Dietary treatments aim to increase fibre and water intake; lifestyle changes involve optimizing toilet posture and time, and avoiding straining.
- Complications are:
- Bloating& abdominal pain: if fibre intake is increased too quickly.
- Worsening of constipation: if insufficient water intake but more fibre.
Biofeedback therapy:
- This therapy works on pelvic floor muscle strength and relaxation during passing bowels.
- Most safe, non-invasive, and effective non-surgical treatment.
- Complications are mostly due to
- Discomfort during first few sessions
- Embarrassment or anxiety of performing well
- Limited effect if there are certain internal blockages in the rectal area.
Pelvic physiotherapy:
- Works on making the pelvic muscles co-ordinate, relax and work together for pushing bowels better.
- Possible complications:
- Muscle soreness from initial sessions
- Frustration as this therapy is a bit slow progressed
Surgical options:
Stapled transanal resection of the Rectum:
- It is also known as the STARR procedure, uses staple device to bring remove any obstructions and bring back the normal shape of the rectal/anal canal
- Complications include
- Most commonly-incontinence or a feeling of increased urgency during bowel movements
- Persisting pain in the pelvic (the entire region just below your waist) region
- Narrowing of the rectal (rectum comes before anus) canal
- Breaking down of the staple line
Rectocele surgery:
- It is also called rectocele repair, it involves surgically repairing the wall between the vagina and rectum.
- Possible complications include:
- Pelvic nerve pain
- Bleeding in this region
- Dyspareunia (painful intercourse)
- Rarely even a rectocele recurrence (condition is same as before surgery again)
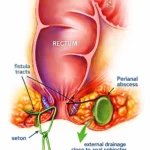
Laproscopic ventral rectopexy:
- This surgery is done to fix the rectal muscles to the tailbone (end bone of the spinal cord-right above the buttocks).
- This option is generally used if there is a “full rectal prolapse” (meaning the rectal canal is slipping out of the final anal hole) or if there are other blockages in the rectal region.
- Possible complications include:
- Sometimes worsened or sometimes newly onset constipation.
- Recurrence of the prolapse (slipping of the rectal canal-making the condition same as before)
- Nerve injury
- Other probable surgical complications like bleeding and infections.
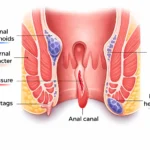
A persistent bump in anus, especially when accompanied by difficulty passing stools, excessive straining, a sensation of incomplete evacuation, or the need for manual assistance during bowel movements, may be associated with obstructed defecation syndrome (ODS), a condition outlined in the Smiles Gastroenterology resource that can involve rectal prolapse, rectocele, or pelvic floor dysfunction and may require targeted medical or surgical treatment to prevent ongoing discomfort and complications.
Dr. Pavithra A is a Senior Colorectal Physician at Smiles Institute of Gastroenterology with over 14 years of clinical experience. Specializing in conditions like piles, fissures, and fistulas, she is particularly recognized for her expertise in treating colorectal issues in women and during pregnancy. Based in Bangalore, Dr. Pavithra is known for her empathetic approach and commitment to providing ethical, patient-centric care for complex digestive and anorectal disorders.