Fistulas are tube-like connections formed in the body in response to long-term infections, to drain infectious fluids out of the body. Anal fistulas are formed in the anal region when pus- filled pockets called perianal abscesses form. They are quite common—especially for those in the age group 30–50 years. It is natural to feel hesitant to ask for help when having fistulas, as the topic itself is a bit awkward. So here is a guide to the whats and whys of fistulas–to help you understand all about it. By the end of this article, you will also understand why talking to your doctor at the early stages is the best step, despite all the fear around this condition.
What is the difference between a simple and complex anal fistula?
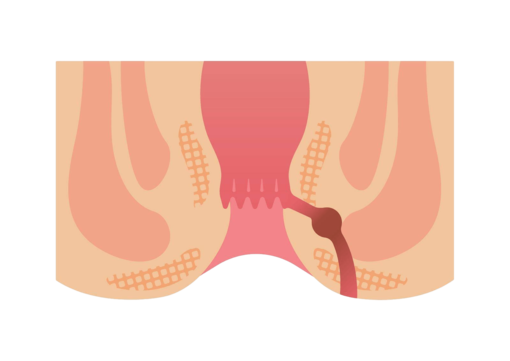
Lining the anal canal, there are many glands which produce mucus. Mucus helps in keeping the passage of stools smooth. When these glands get infected, the pus from them is collected in pockets called abscesses. The body naturally makes drainage tubes from the abscess to the skin surface to release the collected fluids and heal the system.
These drainage tubes are called fistula tracts and can form in many shapes. They can also be just one fistula tract directly to the skin, or this tract—when left untreated—can form multiple branches. Based on these shapes and branching, fistulas are called simple and complex fistulas. Here are some easy-to-understand differences between simple and complex anal fistulas.
| Characteristic | Explanation | Simple fistula | Complex fistula |
| Path of the tract | How the tract is formed in the anal region differs between the two types | It is a simple, straight tunnel/pipe from the abscess to the anus skin. | Has multiple tracks called branches. It looks similar to the root systems of a big tree. |
| Muscle involvement | The sphincter muscle help you control bowel movements. Fistula types differ based on if they involve the sphincter muscles or not. | These are low level fistulas. They pass through minimal or no sphincter muscles. | They are high-level fistulas which go through a significant portion of sphincter muscles. This poses risk during treatment, because cutting sphincter muscles may risk faecal incontinence. |
| Underlying health conditions | A fistula is considered complex if it is linked to underlying factors—irrespective of the tunnel shape. | Formed generally due to untreated perianal abscess. | Fistula due to Crohn’s disease/IBD, recurring fistula, or radiation therapy are considered complex fistulas. |
| Other symptoms | Based on skin holes/openings | Usually one small hole on the anal skin surface. | Has multiple holes in the skin |
| Pain | Generally, is localized to a point, and is a dull throbbing pain. | Can cause deep, and widespread pain in the anal region. | |
| Recurrence | Rarely recurs after surgical removal. | High chances of recurrences if not treated properly. | |
| Drainage | They release pus or blood in small amounts. | May involve heavier release of pus and blood. Sometimes there is release of even faecal matter r gas through the fistula holes. |
Can a fistula be cured permanently with medication alone?
The short answer—no, fistula removal necessarily involves surgical interventions.
Fistula tracts are well-known to remain in the body even after all the liquid drains out. If your doctor has prescribed medications like antibiotics and pain killers, it is for managing the symptoms of the fistula only. Often the fistula is deeply embedded and hence, not accessible to antibiotics. Thus, taking antibiotics for fistula is to keep the infection from spreading to other body parts.
Using other means of relief like sitz baths, and regularly washing the anal area only help to keep the fistula tract clean, and prevent re-infections.
Empty fistula tracts may not necessarily cause any particular symptom like discomfort or pain unless there is an active infection. However, leaving a fistula tract untreated can complicate matters as they branch out and form complex fistulas.
Thus, the only way to remove a fistula is with the help of surgical interventions. The good news is, in 2026, there are painless, and outpatient fistula removal procedures like FiLaC (Fistula-tract Laser Closure) is used to deliver quick but lasting results. Unlike surgical techniques used in the past, FiLaC uses laser energy to seal the tract with pinpoint precision. Such modern options for fistula treatment offer permanent cure with minimal recovery time and energy investments.
Which type of anal fistula has the highest risk of incontinence?
To know the answer to this common question, it is important to understand the different types of fistulas.
Fistula types—simply explained.
This is a very classic grouping of the fistulas, based entirely on whether or not they involve the sphincter muscles in their path. There are two anal sphincter muscles in your body, the external (the ones you voluntarily control) and the internal one (functions automatically). Removal of fistulas which pass though the external sphincters, risk faecal incontinence the most.
- Intersphincteric fistula: This tract passes in between the two sphincter muscle layers, and is closer to the anal opening. It is the most straightforward type of fistula. This can be easily treated by a fistulotomy without any risk of damaging the external sphincter/control muscle.
- Trans-sphincteric fistula: As in the name, the fistula crosses through both the muscle layers, and exits a bit away from the anal opening. Since the external sphincter is also involved, there is a slight risk of incontinence if too much muscle is touched/damaged. However, FiLaC or the laser surgery is quite beneficial here to not do any damage to the sphincters.
- Suprasphincteric fistula: This one is a bit more complicated than the above two. The fistula here loops above the anal sphincter muscle complex and then travels down again to the skin. This is a complex fistula type, involving multiple stages of treatment to first drain the tract, and then close it.
- Extrasphincteric fistula: This is a rare form of fistula, and bypasses the entire sphincter complex. It begins usually higher up in the colon or the rectum, and heads straight down to the skin of the anus. These are caused by inflammatory bowel diseases, or severe trauma to this region. Treatment focuses on fixing the infection source from where the fistula has started.
As you can see, fistula types which involve the external sphincter used for controlling bowel sensation are the most sensitive to treat. While minimal damage to this muscle is easily healed, and allows for 100% bowel control after the procedure, deeper involvement requires specialized care.
Based on these pointers, the extrasphincteric and suprasphincteric fistulas carry the highest risk of incontinence if not handled with advanced, sphincter-saving technology.
What are the red flag symptoms that mean an abscess has become a fistula?
Anal abscess is the pus-filled pocket formed from infected mucosal glands in the anus. Anal abscess can feel like severe throbbing pain near the anus, redness around a hard lump, can also present with fever, and chills.
When the abscess is left untreated for long periods, it turns into an anal fistula by becoming a persistent, non-healing opening, with foul-smelling pus or blood drainage.
Must-know red flag symptoms when anal abscess becomes a fistula
- Persistent drainage: Drainage can be continuous or intermittent with pus, blood, or faecal matter from a small hole near the anus.
- Recurring abscess: The fistula tract remains open which repeatedly allows the bacteria to enter it, this causes reinfection at the same spot.
- Throbbing pain: Throbbing pain which can worsen while sitting, walking, or during bowel movements.
- Skin irritation: Constant redness, and itching caused by the continuous moisture drainage.
- Other infection signs: Due to the infection, fever, chills, and fatigue can occur.
Anal fistulas: the way forward in 2026.
At the end of the day, an anal fistula is a very common issue with many easy and permanent solution in 2026. While the different types and classifications might seem overwhelming, the most important takeaway is about not fearing the term “surgery” as it no longer means a long, painful recovery or a threat to your quality of life. In 2026, the medical field has moved past the “wait and see” approach. With the rise of sphincter-saving laser treatments and highly accurate diagnostics, the goal is to fix the fistula, with as little disruption to your daily routine as possible.
Take your brave step today and visit Smiles Gastroenterology Centres, Bengaluru. Here, the word complex takes a different meaning, with the access to latest surgical equipment, and equally capable expert colorectal doctors. With these resources at your reach, a healthy and confident life is just a consultation away.
Dr. Parameshwara CM is a global authority in Coloproctology and the visionary founder of SMILES Hospitals, with an extraordinary track record of over 50,000 successful surgeries. A true pioneer in the field, he was the first to introduce Advanced Laser Piles Treatment and sophisticated procedures like LIFT, VAAFT, and STARR to Karnataka, revolutionizing the way digestive disorders are treated. He combines surgical precision with state-of-the-art laser technology to offer bloodless, minimally invasive solutions. Call us: +9108099008800 for further help.