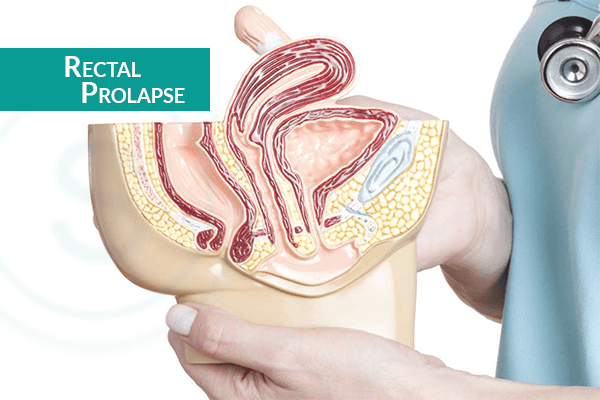
The rectum is the lower part of your colon, where the stool forms. Rectal prolapse occurs when the rectum drops out the body, protruding through the anus. The condition is common in older adults with a history of constipation. The rectal prolapse symptoms include bleeding from the rectum and uncontrolled loss of stool (Bowel Incontinence).
Rectal prolapse causes due to the weakening of sphincter muscles that support the rectum. In the early stages, the prolapse may happen only after a long term strain during a bowel movement. The protruding rectum goes back through the anal canal on its own. Over time, the prolapse may become severe and could require rectal prolapse surgery.
Without treatment, rectal prolapse can be uncomfortable when the rectum will eventually need to be pushed back in manually, says – Dr. Parameshwara C M, the best rectal prolapse doctor in Bangalore.
How is rectal prolapse diagnosed?
Firstly, your doctor will discuss your medical history and perform rectal tests. You may be asked to strain while sitting as if you are having a bowel movement. Being able to see the prolapse helps your doctor to confirm the diagnosis and gives the best treatment.
Rectal Prolapse doctors use several tests to diagnose rectal prolapse which include:
- ● Anorectal manometry: A short pressure-measuring tube inserted inside the rectum to measure how well the anal sphincter muscles are working.
- ● Defecogram: A type of X-ray taken during a bowel movement.
- ● Anal ultrasound: A small probe is inserted into the rectum to take images of the sphincters. This test evaluates the structure and shape of the anal sphincter muscles and surrounding tissue.
- ● Colonoscopy: A flexible tube with a camera inserted inside the rectum so the doctor can do a visual exam.
- ● Barium enema: X-ray images are taken after a type of contrast solution is placed in the rectum.
The experts of rectal prolapse will also evaluate the pelvic floor organs for prolapsed bladder or prolapsed uterus.
What is the treatment of Rectal Prolapse?
If your rectal prolapse symptoms are severe and interfere with your quality of life, you may need surgery.
Our colon and rectal surgeons offer advanced and minimally invasive surgical treatments including:
- ● Rectopexy: A small cut is made through the lower belly and the rectum is attached to the lower part of the backbone to support and keep it in place.
- ● Perineal proctectomy: During this procedure, the surgeon removes the part of the rectum that has prolapsed and joins the ends.
- ● The prolapsed rectum can also be treated by combining these two techniques.
Colorectal surgeons may also recommend non-surgical approaches to prevent rectal prolapse.
- ● High fiber diet
- ● Bowel training
- ● Stool softeners
What are the risk factors of rectal prolapse?
Anyone can develop rectal prolapse, but women over the age of 50 are more likely to have the condition.
Here are some conditions that may increase your risk of prolapsed rectum
- ● Chronic constipation
- ● Straining during bowel movements
- ● Weakened pelvic floor muscles
- ● Childbirth
- ● Chronic Diarrhea
- ● Laxative abuse
- ● Cystic Fibrosis
- ● Aging
What are the complications of rectal prolapse?
The major complications of rectal prolapse include:
- ● The rectum that can’t be manually pushed back into the body. (Incarceration)
- ● The blood supply to the prolapse will be reduced or cut off (Strangulation)
- ● Risk of damage to the rectum, such as bleeding or ulceration.
- ● Death and decay of the strangulated section of the rectum.
- ● The recurrence of the rectal prolapse.
How to manage rectal prolapse after surgery?
After your surgery for rectal prolapse or rectocele, follow these steps for a better and easy recovery.
- ● Avoid activities that increase pressure in your rectal areas like straining during bowel movements or heavy lifting.
- ● Eat at least 3 servings of fresh fruits and vegetables every day. Add high fiber to your diet to prevent constipation.
- ● Drink 6 to 8 glasses of water every day to soften the stools.
- ● Consult your doctor if you notice any unusual symptoms like difficulties with urination, heavy bleeding, fever or chills.
- ● If you are chronically constipated, consult a doctor immediately for better treatment.
- ● Stay active and get regular exercise. If you are obese, work on to get back to a healthy weight.
Do you think you have rectal prolapse? Don’t feel ashamed to consult a doctor. It is imperative to get the right diagnosis for the right treatment.
Our experienced colon and rectal surgeons in Bangalore offer the most advanced and effective approaches for patients with rectal prolapse. You can also opt for Ayurvedic treatment of prolapsed rectum at SMILES to avoid the complications.